Organized by the consortium partner, Universidad de las Palmas de Gran Canaria, and its Fundación Parque Tecnológico, the meeting highlighted the work done in recent months and designed the strategies for the final section of the project.
The afternoon of the first day of the meeting, January 26, 2023, was also marked by the exciting presentation of the project officer appointed by the European Commission. The project officer explained the ongoing work at the European Health and Digital Executive Agency (HaDEA), which is responsible for financing the project, and emphasized the procedures and requirements to opt for funding sources for research from the Commission.
In this sense, the HAPPY PATIENT project officer conveyed the satisfaction of the HaDEA Agency, based in Brussels, for the work developed so far.
Then, the coordination of the project led by the Fundació IDIAP Jordi Gol from Barcelona, took the floor to explain the project’s current state at the level of monitoring the milestones and deliverables delivered to the Commission.
Once the presentation was over, it was time for the University of Copenhagen, which develop the training procedures used in the interventions with the health professionals of the five target countries. Among these resources, the communication tools were highlighted. These communication tools have been translated into several languages, adapted to the local realities of the countries, and made jointly by the university with the collaboration of the consortium and the Spanish Society of Family and Community Medicine, which is also responsible for the communication and dissemination of results.
To end the first day, the workshop «Qualitative studies?» showed that the consortium is really engaged in understanding the reasons behind the results of our First Audit.
On the last day of the meeting, January 27, the Work Package leaders were given a voice and analyzed the data collected by the target countries and interpreted them. In this sense, it should be noted that one of the most remarkable features of HAPPY PATIENT is that this is the first time that a quality-improvement study like this has been carried out on this scale in most care levels (Primary Care, out-of-hours services, nursing homes, and pharmacies).

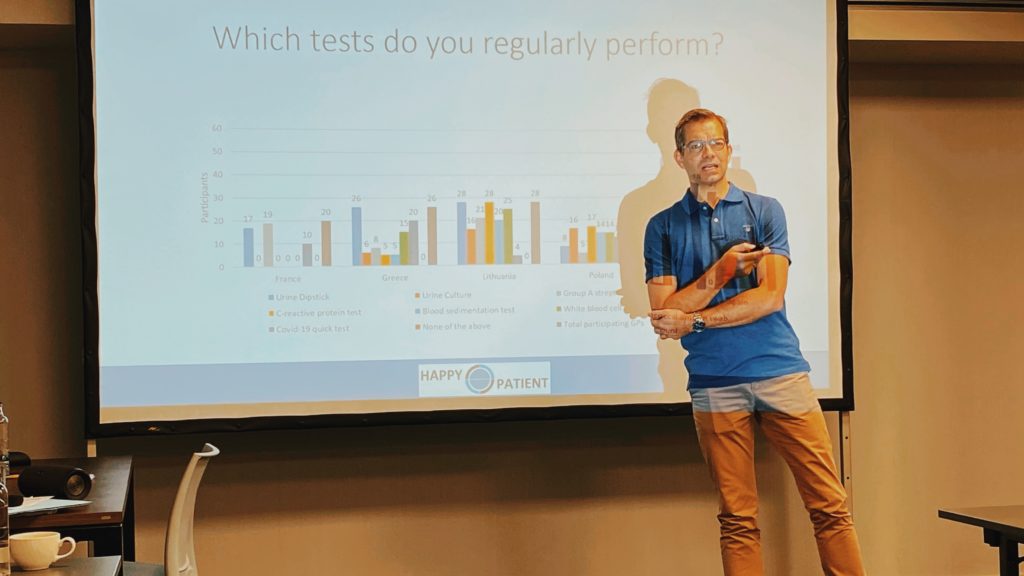
Inspiring was when colleagues from the University of Southern Denmark presented the results of the Audit Cycles. The sum up of the results has been printed and collected in paper format. All the partners have been able to consult the realities observed in the various target countries, and their access to point-of-care tests, which are a tool to reduce unnecessary antibiotics prescription.
Finally, after the interventions of the Norwegian colleagues of the reserach centre NORCE, the Hovedstaden Capital Region, and the University of Groningen – who presented the situation detected in each care level – IDIAP Jordi Gol gave voice to the target countries.
Lithuania, Greece, Spain, Poland, and France explained how the intervention meetings had been organized. All of them were positively surprised by the high level of engagement and attendance rate of their healthcare professionals. «Our face-to-face meeting has facilitated the quality and experience of the intervention», said Ruta Radzeviciene Jurgute from the Lithuanian Mano seimos gydytojas clinic. «In Crete, we used an online platform to deliver the intervention with a high rate of participation», said Christos Lionis from the University of Crete in Greece. In the case of Poland «participants really enjoyed meeting together and also receiving a lecture from a microbiologist who is also a General Practitioner», said Anna Kowalczyk. As for the French partners, they’ve pointed out that the French intervention took place at a national scale in several places in France, and the satisfaction rate was nearly 100%.
In total, over 400 healthcare professionals in Europe are taking in HAPPY PATIENT.
Finally, the meeting hosts, the University of Las Palmas de Gran Canaria, explained the impact and evaluation of the project results, and the Spanish Society of Family and Community Medicine outlined the actions in communication and the strategy for disseminating the final results ever closer.
The second face-to-face meeting of HAPPY PATIENT began right after the kick-off meeting of another European project that also started this week in the Canary Islands. This project is called IMAGINE.
IMAGINE: 8 countries and 320 nursing homes professionals
Overuse of antibiotics in the elderly population contributes to the global health problem of Antibiotic resistance. Hence, it is essential to improve prescribing practices in care facilities for elderly residents. In nursing homes, urinary tract infection (UTI) is the most common reason for Antibiotic prescriptions, but inappropriate medications are frequent. A lack of infection prevention and control (IPC) and wrong diagnosis leads to antimicrobial overprescribing in long-term care facilities (LTCF).
Intense use of antibiotics is reported in long-term care facilities (LTCF) in Europe for treating suspected acute infections. Still, this Antibiotic overprescribing is exceptionally high in suspected urinary tract infections (UTI), leading to a spread of multi-resistant uropathogens.
As a result, critically important broad-spectrum antibiotics are commonly given to residents with these infections, perpetuating the problem of antimicrobial resistance (AMR), which is accompanied by higher morbidity, mortality, and health costs.
European initiatives like the HAPPY PATIENT project – most of whose members are also part of the IMAGINE project – have been highlighting this reality for years in the countries that lead the ranking of unnecessary prescriptions in different settings and levels of care (France, Greece, and
Poland).
International initiatives such as the HAI-Net HALT database have monitored healthcare-associated infections and antimicrobial use in long term care facilities in the EU over the last decade.
And both pieces of research have found that Antibiotic overprescribing, especially those prescriptions that aim to treat Urinary Tract Infections (UTI), is more intense than previously expected in nursing homes.
Pointing in the same direction, there’s the HALT-3 Study on the prevalence of antimicrobial agents, which included 3,052 LTCF in 24 European Union countries between 2016 and 17.
According to the authors, it was evident that 5,035 out of 181,462 eligible residents had received at least one antimicrobial agent on the day of the survey, resulting in a prevalence of antimicrobial use of 5.8%, with Spain and Denmark being the countries with the highest consumption, each.
Nursing homes and antibiotics: Urgent action is needed
European researchers and health professionals see the urgency of taking measures to reduce these numbers and the fact is that for a 1% increase in the proportion of residents over 85 years of age, the prevalence of antimicrobial use increases by 5%.
Prophylactic treatment with antibiotics is generally inappropriate. However, the indication is only reported as a treatment for an acute healthcare-associated infection in 69.5% of the episodes, with prophylaxis accounting for 30% of all the prescribed antimicrobials.
The urinary tract is the most common body site for which antimicrobials are prescribed, with nearly 50% of the cases, followed by infections of the upper and lower airways, accounting for nearly 30% of the antibiotics administered, and infections of the skin and soft tissue in third place.
At least 60% of the antimicrobials prescribed for UTIs are inappropriate. These figures show how, at the present moment, nursing in the European Union is a dangerous breeding ground for the birth of antimicrobial-resistant superbugs. This situation could accelerate the dreaded pandemic of antimicrobial resistance and the fear of a new world where antibiotics will no longer be effective. As in the COVID-19 pandemic, nursing homes can also experience high-risk situations.
The aim of the IMAGINE project is to increase the prevention of infections – mainly UTIs –and reduce Antibiotic inappropriateness for these infections by implementing a multifaceted intervention targeting healthcare professionals (HCP) in LTCFs, including in particular nursing homes.
As in the HAPPY PATIENT, the IMAGINE project applies the Audit Project Odense method of audit and feedback before and after this intervention.
The IMAGINE project will include at least 10 LTCFs in each of the eight participant countries, seven of which are low-income member states, Greece, Hungary, Lithuania, Poland, Slovakia, Slovenia, and Spain.
Denmark will also be participating through its University of Copenhagen and its Capital Region (Region Hovedstaden).
The IMAGINE project will involve 4 nursing home staff professionals (doctors, registered nurses, care assistants, healthcare helpers) in each LTCF in the 8 target countries. Up to 320 nursing home health care professionals (HCP) will be trained in the project.
“By training these 320 HCP we expect to reduce the incidence of suspected UTI by 20% and the antibiotic inappropriateness by 40% for these infections and we also expect a reduction of 10% in the incidence of infections other than UTIs”, says Carl Llor (project’s coordinator and member of the Catalan Health Institute (ICS), the Fundació d’Investigación en Atenció Primària Jordi Gol (IDIAP) and the Spanish Society of Family and Community Medicine).
“The consortium of the IMAGINE project is powerful because each of the partners has a unique profile, bringing its experience and know-how to our mission,” adds Carl Llor.
“Most partners in the IMAGINE project participated in the HAPPY AUDIT project (FP6 2007-2010) and are now participating in the HAPPY PATIENT (3HP 2021-2023)”, says Beatriz González López-Valcárcel, responsible of the Project evaluation and up-scaling at the EU level.
Professor López-Varcárcel explains that this is also important in terms of cost-efficiency because AMR has a substantial economic impact. “AMR cost increases are extremely pessimistic because the problem is growing exponentially. According to the World Bank, in 2030, the global costs attributable to microbial resistance will represent between 1.2% and 4.1% of world GDP.”
During the next 3 years, partners of the IMAGINE project consortium will train nursing home staff in better management and diagnostic of suspected acute infections in 8 target countries.
IMAGINE is an acronym that stands for Improving antibiotic use in long term care facilities by infection prevention and control and antibiotic stewardship.


